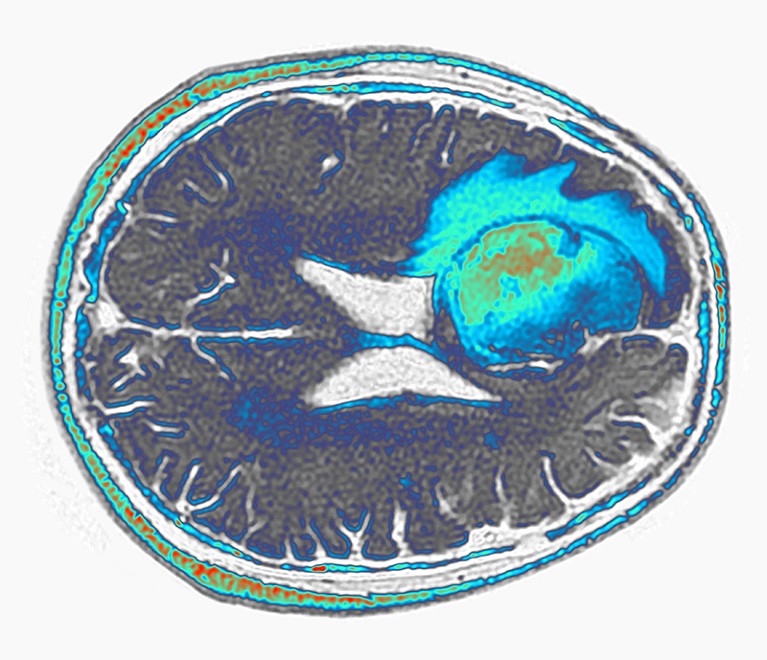
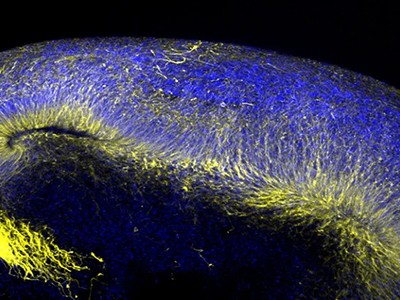
MIT researchers have discovered a brain circuit that drives vocalization and ensures that you talk only when you breathe out, and stop talking when you breathe in.
The newly discovered circuit controls two actions that are required for vocalization: narrowing of the larynx and exhaling air from the lungs. The researchers also found that this vocalization circuit is under the command of a brainstem region that regulates the breathing rhythm, which ensures that breathing remains dominant over speech.
“When you need to breathe in, you have to stop vocalization. We found that the neurons that control vocalization receive direct inhibitory input from the breathing rhythm generator,” says Fan Wang, an MIT professor of brain and cognitive sciences, a member of MIT’s McGovern Institute for Brain Research, and the senior author of the study.
Jaehong Park, a Duke University graduate student who is currently a visiting student at MIT, is the lead author of the study, which appears today in Science. Other authors of the paper include MIT technical associates Seonmi Choi and Andrew Harrahill, former MIT research scientist Jun Takatoh, and Duke University researchers Shengli Zhao and Bao-Xia Han.
Vocalization control
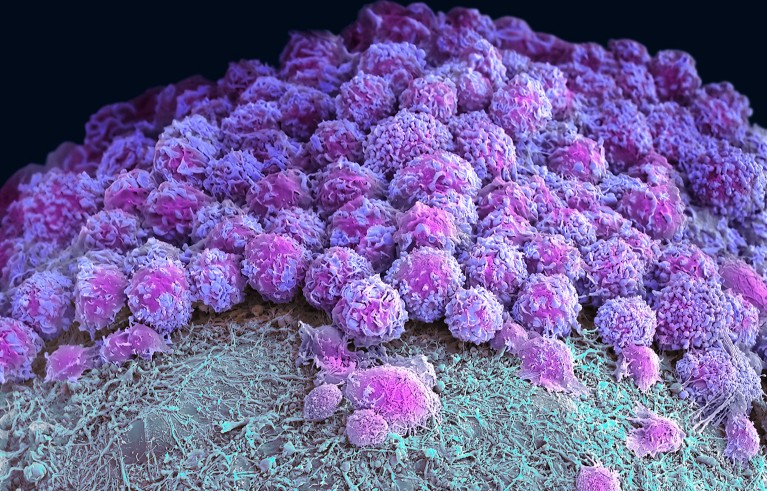
Located in the larynx, the vocal cords are two muscular bands that can open and close. When they are mostly closed, or adducted, air exhaled from the lungs generates sound as it passes through the cords.
The MIT team set out to study how the brain controls this vocalization process, using a mouse model. Mice communicate with each other using sounds known as ultrasonic vocalizations (USVs), which they produce using the unique whistling mechanism of exhaling air through a small hole between nearly closed vocal cords.
“We wanted to understand what are the neurons that control the vocal cord adduction, and then how do those neurons interact with the breathing circuit?” Wang says.
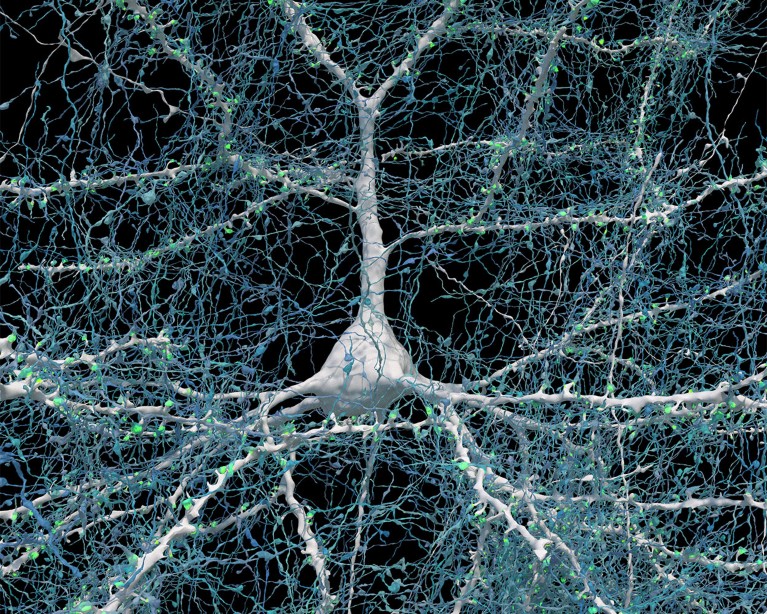
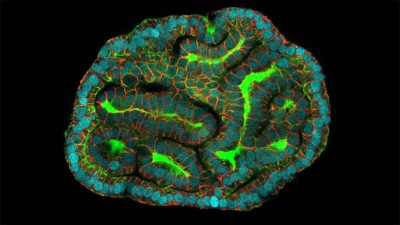
To figure that out, the researchers used a technique that allows them to map the synaptic connections between neurons. They knew that vocal cord adduction is controlled by laryngeal motor neurons, so they began by tracing backward to find the neurons that innervate those motor neurons.
This revealed that one major source of input is a group of premotor neurons found in the hindbrain region called the retroambiguus nucleus (RAm). Previous studies have shown that this area is involved in vocalization, but it wasn’t known exactly which part of the RAm was required or how it enabled sound production.
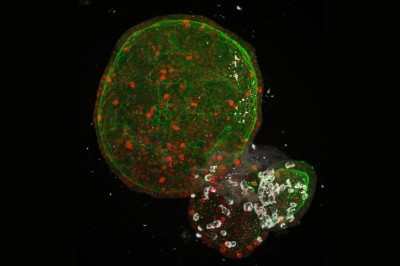
The researchers found that these synaptic tracing-labeled RAm neurons were strongly activated during USVs. This observation prompted the team to use an activity-dependent method to target these vocalization-specific RAm neurons, termed as RAmVOC. They used chemogenetics and optogenetics to explore what would happen if they silenced or stimulated their activity. When the researchers blocked the RAmVOC neurons, the mice were no longer able to produce USVs or any other kind of vocalization. Their vocal cords did not close, and their abdominal muscles did not contract, as they normally do during exhalation for vocalization.
Conversely, when the RAmVOC neurons were activated, the vocal cords closed, the mice exhaled, and USVs were produced. However, if the stimulation lasted two seconds or longer, these USVs would be interrupted by inhalations, suggesting that the process is under control of the same part of the brain that regulates breathing.
“Breathing is a survival need,” Wang says. “Even though these neurons are sufficient to elicit vocalization, they are under the control of breathing, which can override our optogenetic stimulation.”
Rhythm generation
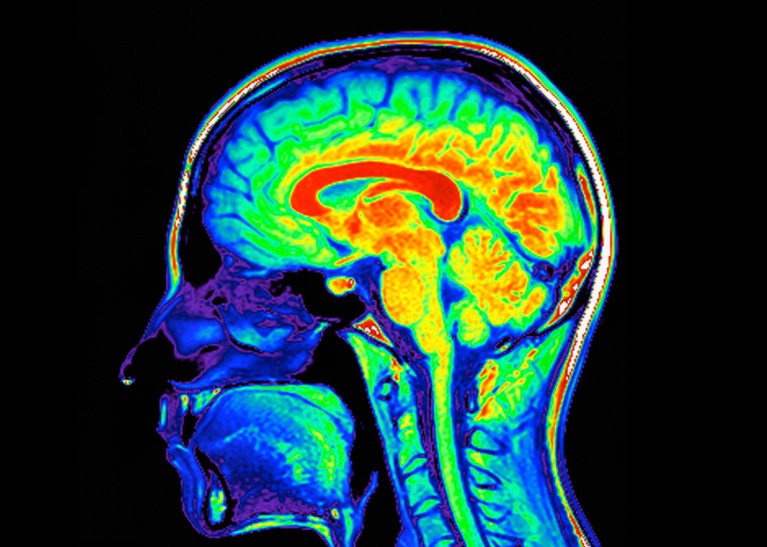
Additional synaptic mapping revealed that neurons in a part of the brainstem called the pre-Bötzinger complex, which acts as a rhythm generator for inhalation, provide direct inhibitory input to the RAmVOC neurons.
“The pre-Bötzinger complex generates inhalation rhythms automatically and continuously, and the inhibitory neurons in that region project to these vocalization premotor neurons and essentially can shut them down,” Wang says.
This ensures that breathing remains dominant over speech production, and that we have to pause to breathe while speaking.
The researchers believe that although human speech production is more complex than mouse vocalization, the circuit they identified in mice plays the conserved role in speech production and breathing in humans.
“Even though the exact mechanism and complexity of vocalization in mice and humans is really different, the fundamental vocalization process, called phonation, which requires vocal cord closure and the exhalation of air, is shared in both the human and the mouse,” Park says.
The researchers now hope to study how other functions such as coughing and swallowing food may be affected by the brain circuits that control breathing and vocalization.
The research was funded by the National Institutes of Health.












.jpg)
.jpg)
.jpg)