[ad_1]
In late 2020, COVID-19’s global death toll was rising as cold weather in the Northern Hemisphere and holiday gatherings spurred rapid transmission of SARS-CoV-2 in the absence of a vaccine. Scientists and public-health officials were desperate for new ways to track the virus, which often moved faster than contact tracers could follow it.
Tong Zhang, an environmental engineer and microbiologist at the University of Hong Kong (HKU), and his colleagues were pioneers of what was fast becoming a popular surveillance method. They had been collecting periodic wastewater samples from about two dozen maintenance holes in the city and testing the sewage for coronavirus DNA, with support from Hong Kong’s government. In late December, they traced an outbreak to a single apartment building where there had been no sign of cases1.
The government quickly took action. Officials tested all of the building’s 2,000-odd residents; 9 tested positive. “Those people were isolated and went to a quarantine site. So they stopped the transmission chain,” Zhang says. After that success, he and his colleagues expanded their efforts.
These scientists traced a new coronavirus lineage to one office — through sewage
Wastewater testing remains part of Hong Kong’s COVID-19 strategy to this day. Zhang’s team tests for the coronavirus at about 20 sites across the city each week, he says, and the team has expanded the analysis of these samples to cover other pathogens, including influenza, rotavirus, norovirus and mpox, as well as markers of antimicrobial resistance. He views wastewater testing as a way to gauge the health of an entire community at once. “If we can make the methodology more standardized”, this tool becomes a “promising and exciting” way to screen the world for pathogens, including those that scientists haven’t yet identified,he says.
Many researchers are following similar approaches. There are currently more than 4,600 sites around the world where wastewater is being collected for SARS-CoV-2 testing, and some of the research teams involved are investigating other potential applications, such as tracking illicit drug use and even the prevalence of cancer.
But whether this has the potential to be an effective public-health strategy is still a matter of debate. Leo Poon, a colleague of Zhang’s at HKU’s School of Public Health, says that more research should be done before health agencies expand their sewage testing programmes and make this surveillance part of their routine budgets. “There’s still a lot unknown,” he says, particularly in terms of testing for pathogens besides SARS-CoV-2. “I think there’s a steep learning curve at the moment: when we detect something, what does it mean?”
Early accomplishments
Many of the projects tracking COVID-19 through wastewater started in similar ways. Scientists learnt early in the pandemic that SARS-CoV-2 could be identified in sewage2, and made contact with local water authorities and health agencies to get samples.
By the end of 2020, several studies had shown that levels of coronavirus in public water systems could correlate with the number of COVID-19 cases in the community. For example, researchers at Stanford University in California found that viral levels in wastewater rose and fell with cases in the San Francisco Bay area3. The group that led the work has gone on to found the WastewaterSCAN project, which tests samples from nearly 200 sites across the United States (see ‘Peak transmission’).
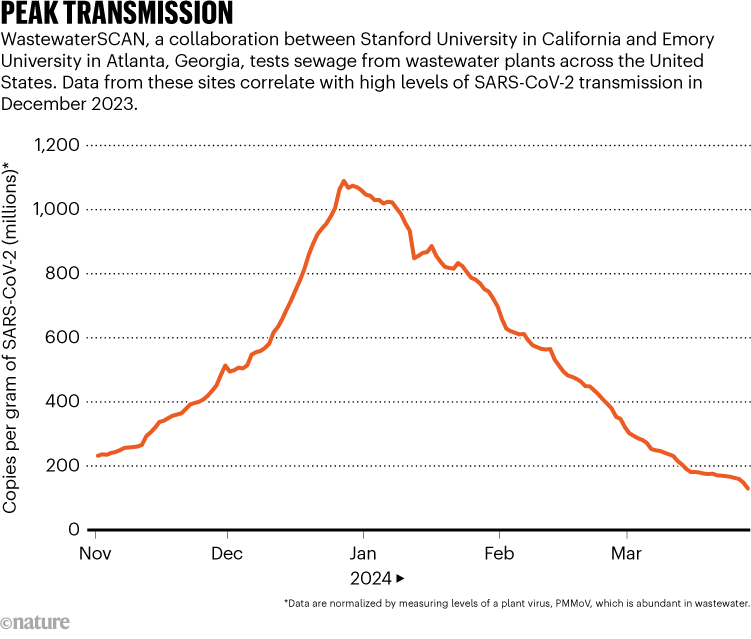
Source: WastewaterSCAN
In the most successful wastewater projects, scientists say, researchers collaborated directly with public-health officials, who used the data to inform COVID-19 safety policies. This happened in rural parts of Ghana, where, as in Hong Kong, wastewater testing found COVID-19 cases that hadn’t been caught by other types of surveillance. Habib Yakubu, a public-health researcher at Emory University’s Center for Global Safe Water, Sanitation, and Hygiene in Atlanta, Georgia, worked with a team of Ghanaian scientists to develop testing methods that accounted for the country’s limited public sewers and laboratory equipment. They tried this in two rural districts, Nanumba North and Mion, where government officials suspected that COVID-19 might be spreading but where clinical testing hadn’t identified any cases.
The researchers worked with community leaders to identify sites for sampling, including schools, health-care facilities, markets and streams used for washing clothes. “We looked at, where do people converge?” Yakubu says. COVID-19 was, in fact, present in these regions, the researchers found. As a result, officials increased public-health activities, including community education and vaccination efforts. The team tested for other diseases that are common in Ghana, including cholera and typhoid, which has also informed health actions.
For scientists at the Tata Institute for Genetics and Society in Bengaluru, India, the need for wastewater testing for COVID-19 became clear after the country’s devastating wave of the Delta variant of SARS-CoV-2 in early 2021, says Farah Ishtiaq, an evolutionary ecologist at Tata who leads the COVID-19 surveillance programme in the city. She and her colleagues worked with officials to set up testing at 28 water treatment plants in Bengaluru — a logistically challenging task, because the team had to collect samples manually rather than using the automated samplers common in higher-income nations.
This testing proved its worth during the spread of the Omicron variant in Bengaluru the following year, Ishtiaq says. Wastewater data demonstrated that Omicron variants were spreading widely across the city at a time when data from the health-care system were limited. Officials responded by renewing mask mandates and placing restrictions on large gatherings, she says.
Inspired by case studies such as these, the field has grown drastically over the past 4 years, with hundreds of research teams now testing in 72 countries, according to the COVIDPoops19 dashboard maintained by environmental engineer Colleen Naughton and her colleagues at the University of California, Merced (see ‘Uneven coverage’).
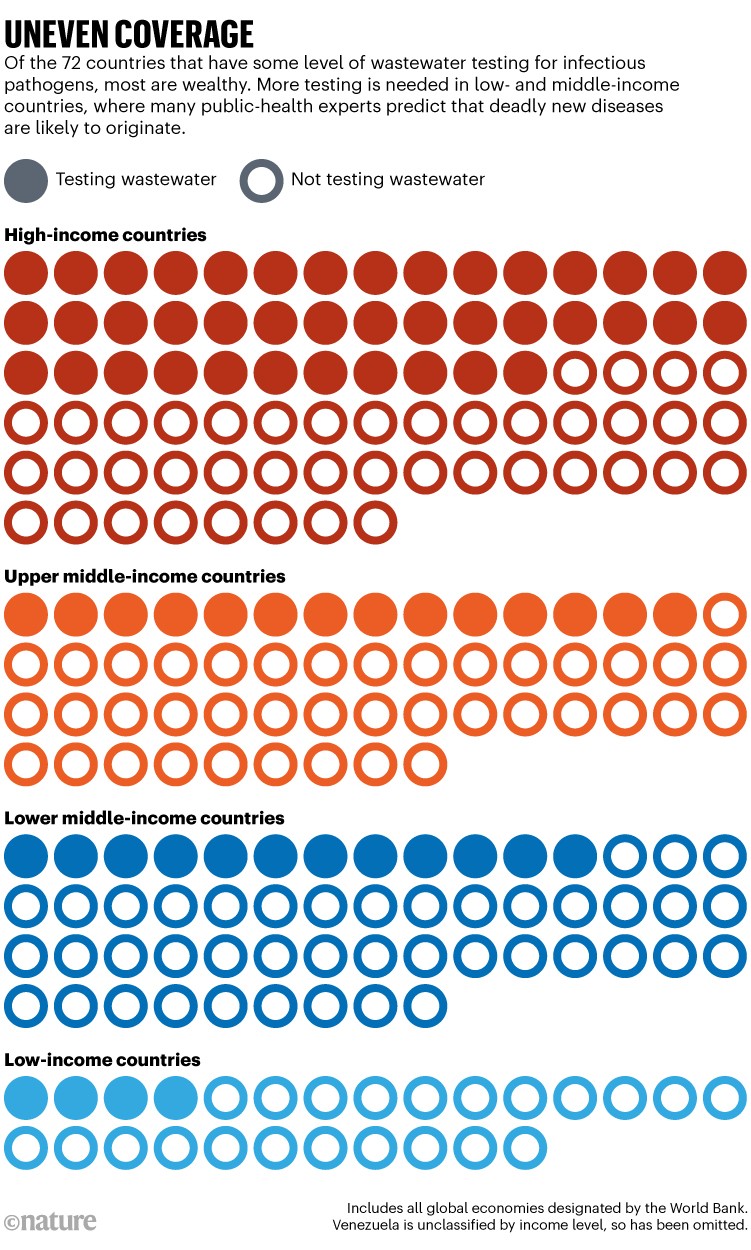
Sources: COVIDPoops19 (https://go.nature.com/4ATGHY)/World Bank
Interpreting poo
In December 2023 and January 2024, it was clear that COVID-19 was spreading widely in several parts of the world. But public-health agencies had severely cut back on conventional testing and surveillance programmes, leading to uncertainty about how much the coronavirus was spreading, and a sudden focus on wastewater-based epidemiology.
Some scientists and social-media commentators stated that SARS-CoV-2 levels in wastewater correlated with specific case numbers, estimating huge surges in the United States and Europe. But others cautioned that wastewater surveillance is not reliable enough to predict true infection numbers. There’s a “false sense of precision” in such estimates, says Sam Scarpino, an epidemiologist at Northeastern University in Boston, Massachusetts, who has worked on COVID-19 data systems.
Estimates are difficult to make because the sewage data differ considerably from conventional health indicators. In typical surveillance, data represent individual infected people who can be identified through contact tracing, isolated and treated. In wastewater surveillance operations, data can represent entire communities.
COVID variants found in sewage weeks before showing up in tests
They make “a litre represent a million people”, says Douglas Manuel, a public-health physician at the University of Ottawa in Canada. Manuel and his colleagues have identified several variables that can alter results from such screenings; these include population density, precipitation, sample composition, handling and testing methods and quality-control measures4. For example, as snow melts in Ottawa’s spring, it flows into the wastewater system and “scours out” solid waste that might have built up in the pipes, Manuel says. This could interfere with findings relating to SARS-CoV-2 measurements.
To account for those variables, researchers tend to compare measurements from one site over time. The US Centers for Disease Control and Prevention (CDC), for instance, developed a metric called the wastewater viral activity level that compares a testing site’s recent SARS-CoV-2 measurement to past ones, then averages those comparison values across larger regions.
These comparison metrics can be helpful for presenting wastewater results to the public, but they gloss over the data’s complexity. Bilge Kocamemi, an environmental engineer at Marmara University in Istanbul and a project coordinator for Turkey’s wastewater testing, says that she quickly realized that “scientific representation of the data makes the data unusable for the public”. Instead, she and her colleagues developed a relatively simple COVID-19 map: testing sites are displayed in different shades of yellow and green, depending on how high SARS-CoV-2 levels are. This coloured scale is not precise, Kocamemi says, but it’s easy for people who don’t have a scientific background to understand.
Improving estimates
Modelling case counts — or other metrics of COVID-19 spread in a community, such as how many people will be hospitalized — from viral levels in wastewater is difficult, but not impossible, say scientists who work on this challenge. Such models would make it easier for health officials to make policy decisions on the basis of sewage data.
The myriad ways sewage surveillance is helping fight COVID around the world
The CDC’s Center for Forecasting and Outbreak Analytics in Washington DC, which launched in 2022, is one group taking on this challenge. Wastewater data are “a really good leading indicator” for COVID-19’s burden on hospitals, says Dylan George, the centre’s director. In February, George and his colleagues released new hospital forecasting models informed by wastewater data, among other metrics (see go.nature.com/43xumbz). Studies have shown that such models are more accurate when they use wastewater data in tandem with data from the health-care system, rather than just one of those sources5.
George cautions that ongoing research will be needed to better understand the connection between virus levels in wastewater and disease levels in a community. For example, some scientists think that virus levels might change as SARS-CoV-2 continues to mutate; a variant known as JN.1 might cause people to shed more virus particles, or shed them for longer compared with previous variants, George says. “I think that’s going to be an active area of research going forward.”
Modellers would like to have more detailed clinical testing data to allow them to make better comparisons between wastewater results and community infections. The challenge is often even greater for researchers testing wastewater for other viruses, says Casandra Philipson, a scientist at Ginkgo Bioworks, a company in Boston that analyses sewage from aeroplanes and airports, along with conducting research into new biosecurity tools. Philipson says that there are decent clinical data available for COVID-19, flu and respiratory syncytial virus. But, she adds, “When you get outside of those three pathogens, there really is a massive data scarcity issue.”
What else can be tested in sewage?
Some scientists are interested in a range of other diseases and health indicators that show up in people’s waste.

Manual wastewater sampling in India.Credit: Environmental Images/Universal Images Group/Shutterstock
Bernd Manfred Gawlik, who coordinates wastewater work at the European Commission’s Joint Research Centre in Brussels, calls wastewater the “dirty blood of the city”, and compares sewage sampling to blood testing. “We are now only starting to understand” how to diagnose this “blood” at the collective level, he says.
One common target of testing is antimicrobial resistance (AMR), an area of wastewater research that pre-dates the pandemic. Ishtiaq, in Bengaluru, says that “AMR is a huge problem in this part of the world”, because many people use unregulated antibiotics. Her research has expanded from COVID-19 testing to a multifaceted, genomic platform that can look for both viral and bacterial infections. Wastewater data will help researchers to understand which pathogens are driving infections and communicate that information to physicians, she says.
Fatma Guerfali, a molecular biologist and bioinformatician at the Pasteur Institute in Tunis, is also tracking AMR in Tunisia, one of the countries considered most at risk. Guerfali says that she and her colleagues are working with the country’s health agency, as well as with research collaborators in other African countries, to determine how best to expand the programme, which started with COVID-19 testing.
How sewage could reveal true scale of coronavirus outbreak
Beyond global targets such as AMR and flu, wastewater testing priorities differ according to local health challenges. Because this testing can pick up a wide variety of pathogens, scientists often consult with health agencies to determine which targets to prioritize. In Louisville, Kentucky, for example, Ted Smith, director of the Center for Healthy Air, Water and Soil at the University of Louisville, and his colleagues are testing for a ‘panvirome panel’ that includes about 30 pathogens of interest to the local health agency. Last year, the testing picked up measles during an outbreak in the state, and health officials used the data to inform vaccination programmes, alerts for physicians and other health efforts, he says.
Another area of expansion lies in testing chemicals that people excrete into wastewater. Some researchers, such as those at the start-up company Biobot Analytics in Cambridge, Massachusetts, are screening for opioids and other drugs with a risk of misuse. Smith and his colleagues are testing sewage for compounds indicative of exposure to air pollution and they have started research into lead levels. “Every day, we come up with new things that we can interrogate wastewater for,” he says.
A few researchers are even going beyond diseases spread by humans to those spread by animals. In 2022, scientists published work linking new SARS-CoV-2 variants in New York City’s wastewater to the city’s rats6. Ishtiaq is looking at avian flu in Bengaluru, and Ekta Patel, a scientist at the International Livestock Research Institute in Kenya, is studying animal diseases there.
Patel and her colleagues are sampling sewage at slaughterhouses and testing for 66 pathogens, including anthrax, brucellosis, and Rift Valley fever. To complement the wastewater tests, Patel hopes her team can collect data from veterinary clinics and community hospitals.
Some wastewater scientists reflect on how different the early days of the COVID-19 pandemic might have been had there been a robust global sewage-surveillance system in place. Researchers could have “immediately retroactively screened wastewater all around the planet” as soon as the virus’s sequence was released, Scarpino says. This screening could have led to a global list of places SARS-CoV-2 was already spreading, informing strategies to contain the virus even before clinical testing was widely available.
Scarpino argues that such a system would require major financial investment, national and scientific leaders who can take ownership of those projects and standards that make wastewater data more comparable across countries7.
The current COVID-19-testing community “came out of need and chaos”, says Megan Diamond, who works on wastewater surveillance at the Rockefeller Foundation in New York City. Global and regional institutions such as the World Health Organization, the European Union and the Africa Centres for Disease Control and Prevention might need to step up and offer guidance for testing, data sharing and standards, Diamond says.
Gawlik has worked on one such broad effort: the Global Consortium for Wastewater and Environmental Surveillance for Public Health, or GLOWACON, which was launched in Brussels in March. By recruiting more than 300 collaborators from around the world, including scientists, government officials and representatives of international organizations, to this consortium, he hopes to advance new methods for diagnosing health issues from the “dirty blood” of cities around the world.
[ad_2]
Source Article Link