[ad_1]
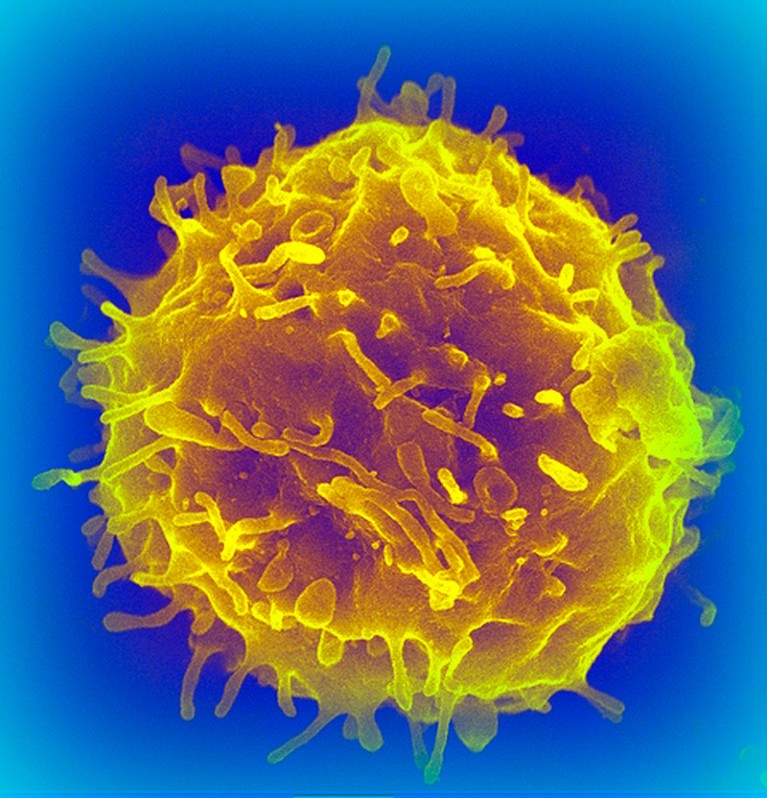
Blood stem cells (example pictured; artificially coloured) generate red blood cells and immune cells.Credit: Science Photo Library
Old mice developed more youthful immune systems after scientists reduced aberrant stem cells in the aged animals1. The technique strengthened the old rodents’ responses to viral infection and lowered signs of inflammation.
The approach, published on 27 March in Nature, treats older mice with antibodies to diminish a population of stem cells that give rise to a variety of other cell types, including those that contribute to inflammation. Excess inflammation can wreak havoc in the body, and these pro-inflammatory stem cells become dominant as mice and humans age.
It will be years before the approach can be tested in people, but many aspects of the stem-cell biology that underlies immune-cell production are similar between mice and humans. “It’s a really important first step,” says Robert Signer, a stem-cell biologist at the University of California, San Diego, who was not involved in the research. “I’m excited to see where they take this work next.”
Skewed immune system
For decades, researchers in Irv Weissman’s group at Stanford University in California have painstakingly tracked the fate of blood stem cells. These replenish the body’s stores of red blood cells (which carry oxygen from the lungs to all parts of the body) and white blood cells (which are key components of the immune system).
Pregnancy advances your ‘biological’ age — but giving birth turns it back
In 2005, Weissman and his colleagues found that populations of blood stem cells shift as mice age2. In young mice, there is a balance between two types of blood stem cell, each of which feeds into a different arm of the immune system. The ‘adaptive’ arm produces antibodies and T cells targeted to specific pathogens; the ‘innate’ arm produces broadbrush responses, such as inflammation, to infection.
In older mice, however, this balance becomes skewed towards the pro-inflammatory innate immune cells. Similar changes have been reported in the blood stem cells of older humans, and researchers speculate that this could lead to a diminished ability to mount new antibody and T-cell responses. That might explain why older people are more prone to serious infections from pathogens such as influenza viruses and SARS-CoV-2, and why they have weaker responses to vaccination than younger people do.
Restoring the balance
If that were the case, then restoring balance to the populations of blood stem cells could also rejuvenate the immune system. The team tested this by generating antibodies that bind to the blood stem cells that predominantly generate innate immune cells. They then infused these antibodies into older mice, hoping that the immune system would destroy the stem cells bound by the antibodies.
The antibody treatment rejuvenated the immune systems of the treated mice. They had a stronger reaction to vaccination, and were better able to fend off viral infection, than older mice who had not received the treatment. The treated mice also produced lower levels of proteins associated with inflammation than did old, untreated mice.
First hint that body’s ‘biological age’ can be reversed
This is an important demonstration that the different populations of blood stem cells influence how the immune system ages, says Signer.
But it’s also possible that the antibody treatment did more than just affect the dominant blood stem cell population, says Enca Montecino-Rodriguez, who studies the development of white blood cells at the David Geffen School of Medicine at the University of California, Los Angeles. The treatment might also affect the environment in which the blood stem cells live. Or it could clear other aged cells from the body, or trigger immune responses that affect how the mice respond to vaccines and viruses, she says.
Weissman says that his team is working on a similar approach to rebalance aged human blood stem cells. But even assuming ample funding and no unexpected setbacks, it will be at least three to five years before they can begin testing it in people, he says.
In the meantime, his team will continue to study mice to learn more about other effects of the antibody therapy, such as whether it affects the rates of cancer or inflammatory diseases. “The old versus the young blood-forming system makes a big deal of difference,” says Weissman. “It’s not just a difference in the bone marrow. It’s a difference all over the body.”
[ad_2]
Source Article Link



