[ad_1]
In 2010, Theresa Chaklos was diagnosed with chronic lymphocytic leukaemia — the first in a series of ailments that she has had to deal with since. She’d always been an independent person, living alone and supporting herself as a family-law facilitator in the Washington DC court system. But after illness hit, her independence turned into loneliness.
Loneliness, in turn, exacerbated Chaklos’s physical condition. “I dropped 15 pounds in less than a week because I wasn’t eating,” she says. “I was so miserable, I just would not get up.” Fortunately a co-worker convinced her to ask her friends to help out, and her mood began to lift. “It’s a great feeling” to know that other people are willing to show up, she says.
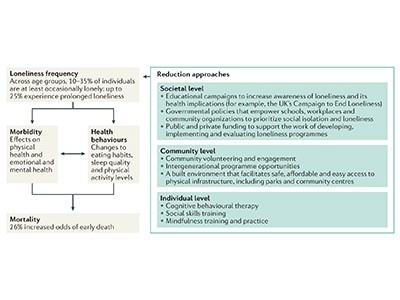
Many people can’t break out of a bout of loneliness so easily. And when acute loneliness becomes chronic, the health effects can be far-reaching. Chronic loneliness can be as detrimental as obesity, physical inactivity and smoking according to a report by Vivek Murthy, the US surgeon general. Depression, dementia, cardiovascular disease1 and even early death2 have all been linked to the condition. Worldwide, around one-quarter of adults feel very or fairly lonely, according to a 2023 poll conducted by the social-media firm Meta, the polling company Gallup and a group of academic advisers (see go.nature.com/48xhu3p). That same year, the World Health Organization launched a campaign to address loneliness, which it called a “pressing health threat”.
But why does feeling alone lead to poor health? Over the past few years, scientists have begun to reveal the neural mechanisms that cause the human body to unravel when social needs go unmet. The field “seems to be expanding quite significantly”, says cognitive neuroscientist Nathan Spreng at McGill University in Montreal, Canada. And although the picture is far from complete, early results suggest that loneliness might alter many aspects of the brain, from its volume to the connections between neurons.
Subjective and contagious
Loneliness is a slippery concept. It’s not the same as social isolation, which occurs when someone has few meaningful social relationships, although “they’re two sides of the same coin”, says old-age psychiatrist Andrew Sommerlad at University College London. Rather, loneliness is a person’s subjective experience of being unsatisfied with their social relationships.
The list of health conditions linked to loneliness is long and sobering1 (see ‘Loneliness and health’). Some of these make intuitive sense — people who feel lonely are often depressed, for example, sometimes to the point of being at risk of suicide. Other links are more surprising. Lonely people are at greater risk of high blood pressure and immune-system dysfunction compared with those who do not feel lonely, for example. There’s also a startling connection between loneliness and dementia, with one study reporting that people who feel lonely are 1.64 times more likely to develop this type of neurodegeneration than are those who do not3.
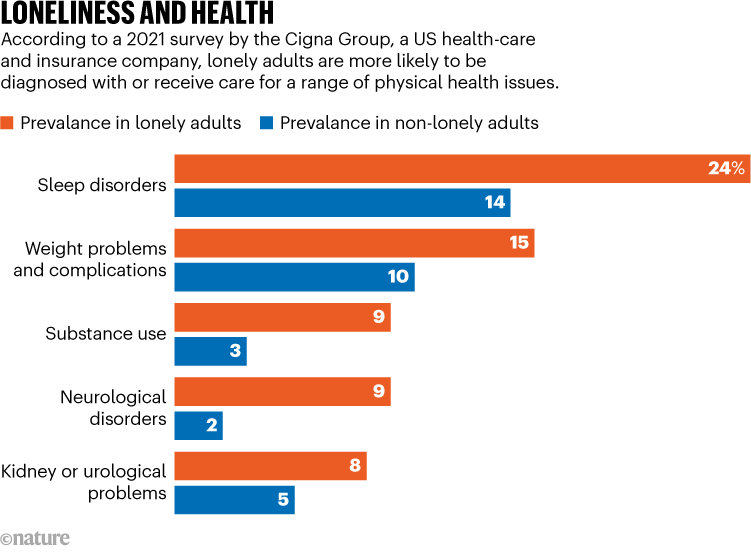
Source: The Cigna Group
A number of physiological effects, including the ability to sleep, increased stress-hormone levels and increased susceptibility to infections, could link loneliness with health problems. But the way in which these factors interact with one another makes it difficult to disentangle the effects of loneliness from the causes, cautions cognitive neuroscientist Livia Tomova at Cardiff University, UK. Do people’s brains start functioning differently when they become lonely, or do some people have differences in their brains that make them prone to loneliness? “We don’t really know which one is true,” she says.
Whatever the cause, loneliness seems to have the biggest effect on people who are in disadvantaged groups. In the United States, Black and Hispanic adults, as well as people who earn less than US$50,000 per year, have higher rates of loneliness than do other demographic groups by at least 10 percentage points, according to a 2021 survey by the Cigna Group, a US health-care and insurance company (see go.nature.com/43eakds). That’s not surprising because “loneliness, by definition, is an emotional distress that wants us to adapt our social situations”, says geriatrician and palliative-care physician Ashwin Kotwal at the University of California, San Francisco. Without financial resources, adapting is harder.
The COVID-19 pandemic might have exacerbated loneliness by forcing people to isolate for months or years, although “that data is still emerging”, Kotwal says. Older adults have long been thought of as the demographic most heavily affected by loneliness, and indeed it is a major problem faced by many of the older people that Kotwal works with. But the Cigna Group’s data suggest that loneliness is actually highest in young adults — 79% of those between the ages of 18 and 24 reported feeling lonely, compared with 41% of people aged 66 and older.
Loneliness eats at you
A growing amount of research is exploring what happens in the brain when people feel lonely. Lonely people tend to view the world differently from those who aren’t, says cognitive neuroscientist Laetitia Mwilambwe-Tshilobo at Princeton University in New Jersey. In a 2023 study, researchers asked participants to watch videos of people in a variety of situations — for example, playing sports or on a date — while inside an magnetic resonance imaging scanner4. People who did not report being lonely all had similar neural responses to each other, whereas the responses in people who felt lonely were all different — from the other group and from each other. The authors hypothesized that lonely people pay attention to different aspects of situations from non-lonely people, which causes those who feel lonely to perceive themselves as being different from their peers.
Feeling lonely in research? You’re not alone
This would mean that loneliness can feed back on itself, becoming worse over time. “It’s almost like a self-fulfilling prophecy,” Mwilambwe-Tshilobo says. “If you think that you’re lonely, you’re perceiving or interpreting your social world more negatively. And that makes you move further and further away.” Some studies have shown that this effect can spread through social networks, giving loneliness a contagious quality5.
Historically, staying close to others was probably a good survival strategy for humans. That’s why scientists think that temporary loneliness evolved — to motivate people to seek company, just as hunger and thirst evolved to motivate people to seek food and water.
In fact, the similarities between hunger and loneliness go right down to the physiological level. In a 2020 study, researchers deprived people of either food or social connections for ten hours. They then used brain imaging to identify areas that were activated by images of either food — such as a heaping plate of pasta — or social interactions, such as friends laughing together. Some of the activated regions were unique to images either of food or of people socializing, but a region in the midbrain known as the substantia nigra lit up when hungry people saw pictures of food and when people who felt lonely saw pictures of social interactions6. That’s “a key region for motivation — it’s known to be active whenever we want something”, says Tomova, who is an author on the study.
More links are emerging between loneliness and how the brain processes feelings of reward. In mice, loneliness sensitizes certain midbrain neurons to a neurotransmitter called dopamine7, which can also cause people to cave in to cravings, such as for food and drugs. Likewise, isolation might make humans more sensitive to rewards and more eager to seek them out. In 2023, Tomova and her colleagues published a preprint8 for a study in which they isolated adolescents from social contact for up to four hours. After isolation, participants were offered the chance to earn a monetary reward. The isolated participants agreed more quickly than did those who were not isolated, suggesting that isolation had made them more responsive to rewarding actions.
Loneliness and health
Although research on dopamine and loneliness is still emerging, scientists have also long recognized the connection between loneliness and another type of chemical signal — stress hormones called glucocorticoids. Humans need some level of glucocorticoids “to function; to wake up”, says neurophysiologist John-Ioannis Sotiropoulos at the National Centre for Scientific Research ‘Demokritos’ in Athens. But persistent loneliness leads to chronically high levels.
These chemicals could provide a link between loneliness and dementia. In a mouse model of Alzheimer’s disease, for example, glucocorticoids increased the levels of two proteins that are involved in the main hallmark of the condition, the protein plaques that tangle around neurons and interfere with memory and cognition9.
Stress is an extra assault on brains that are already wearing out as people get older, Mwilambwe-Tshilobo says, but she wants to see more research before committing to an opinion on exactly what part stress-related chemicals play in neurodegeneration. “It could accelerate the rate of ageing, but there hasn’t been work that explicitly looks at that,” she says.
Tomova says that although high levels of stress hormones probably contribute to dementia, it’s also likely that people who feel lonely miss out on the mental exercise that social interactions provide. And just as a muscle needs exercise to stay fit, so does the brain. In fact, loneliness has been associated with a smaller volume of grey matter in the brain10. “This is all hypothesis, really, at this stage,” Sommerlad says, but the idea is that socializing maintains neural connections that might otherwise be lost.
Turning inward
Researchers looking for the neural signature of loneliness have also found differences that could help to explain some of the correlations between loneliness and dementia. Previous research has suggested that there are changes in the connectivity between brain areas in people who feel lonely11. A 2020 study12 examined an area of the brain called the default network — so called because it’s active by default when a person isn’t engaged in a particular task and turns their attention inward — in older people who reported being lonely.
The hurt of loneliness and social isolation
Previous work had suggested that young people who feel lonely have high neural cross-talk between the default network and other networks associated with vision, attention and executive control13, possibly because they’re on high alert for social cues, says Spreng, one of the authors on the 2020 study of older people. But his team found the opposite in brain scans from the UK Biobank cohort of people aged 40 to 69. Loneliness weakened connections between the default network and the visual system and instead strengthened connections within the default network.
That could be because older people remedy loneliness by retreating into memories of past social experiences, Spreng says. In doing so, they strengthen the default network.
The default network is one of many networks in the brain that accrues damage during Alzheimer’s disease. Spreng and his colleagues are investigating whether strong default networks can indeed be linked to neurodegeneration — and if so, why. He wonders whether robust neural connections might allow pathologies to spread more readily in the network. The idea is far from proven, but it’s a plausible explanation and “an interesting hypothesis”, says cognitive neuroscientist Anastasia Benedyk at the Central Institute of Mental Health in Mannheim, Germany.
The study “lays the foundation for us to be able to test some hypotheses a little bit more empirically”, says Mwilambwe-Tshilobo, who was also involved in the work linking the default network with loneliness.
Finding solutions
Some remedies for loneliness will come as no surprise. Increasing access to social activities, for example by housing people in communities with common areas, can help, Sommerlad says. Some researchers are also finding ways to tap into the neural mechanisms underlying loneliness directly, through exercise, for instance.
Walking 4–5 kilometres over the course of an hour completely reversed feelings of low mood associated with loneliness in some people, Benedyk and her colleagues found14. What’s more, people with high connectivity in their default networks — the same area Spreng studied, which is also known to be affected by depression — were among those who benefited from exercise the most.
One possible explanation for this observation is that people with depression are “stuck in rumination” — a behaviour that draws heavily on the default network, Benedyk says. Exercise could force them to use other parts of their brain by interrupting neural processes that are associated with self-reflection and shifting activity to areas associated with physical activities — freeing them from a cycle of negative thoughts.
Exercising is also a great excuse to socialize. These days, Chaklos is retired, but she now leads the Boston branch of a US programme called ‘Walk with a Doc’, in which physicians invite community members to walk with them. At the group’s February walk, about 14 people chatted and strolled inside the Prudential Center mall in Boston, Massachusetts, where they could avoid New England’s winter weather. The activity “just uplifts a person’s mood”, Chaklos says. “Even if you’re still going back home to be by yourself, you don’t feel totally alone any more.”
[ad_2]
Source Article Link