[ad_1]
Hello Nature readers, would you like to get this Briefing in your inbox free every day? Sign up here.

Jaime Guevara-Aguirre (back left) and Valter Longo (back right) pose with several of the Laron study participants.Credit: Courtesy Jaime Guevara-Aguirre & Valter Longo
People with Laron syndrome — a growth-hormone-receptor condition — seem to be at lower risk of developing cardiovascular disease than relatives who do not have the syndrome. Laron syndrome had already been linked to health benefits including protection against diabetes, cancer and cognitive decline. “They seem to be protected from all the major age-related diseases,” says biogerontologist Valter Longo, a co-author on the cardiovascular study. It’s unclear if people with Laron syndrome live longer on average than those without it, but mice with a similar condition live for about 40% longer than do control animals.
The H5N1 strain of avian influenza has been spreading undetected in US cattle for months, according to a preliminary analysis of genomic data released by the US Department of Agriculture. The outbreak is likely to have begun when the virus jumped from an infected bird into a cow, probably around late December or early January. But the publicly released data do not include critical information that would shed light on the outbreak’s origins and evolution. “In an outbreak response, the faster you get data, the sooner you can act,” says genomic epidemiologist Martha Nelson. “Whether we’re not too late, to me, that’s kind of the million dollar question.”
On the outskirts of Beijing, researchers from all over the world have come together at the Synergetic Extreme Condition User Facility to push matter to its limits with extreme magnetic fields, pressures and temperatures, and examine it in new ways with extremely precise resolution in time. One particularly tantalizing goal for many researchers using this US$220-million toolbox is to discover new superconductors, materials that conduct electricity without resistance. Nature reporter Gemma Conroy steps inside to take a look.
Features & opinion
Climate change is completely reshaping the ecosystem in one of the best-studied Arctic fjords, on the northwest side of the Norwegian archipelago Svalbard. Since the inlet stopped freezing over during the winter, Arctic mammals such as beluga whales have left and more southerly animals including Atlantic puffins have moved in. New habitats have popped up along the shoreline where sea ice once suffocated plant growth. “It’s incredible that I — in my time — have been able to see such dramatic changes,” says ecotoxicologist Geir Wing Gabrielsen.
“Lots of our members call us ‘the magic money tree’,” says Alison Baxter, head of communications for the Authors’ Licensing and Collecting Society (ALCS), a UK agency that compensates authors when their works are copied or shared after publication. Such societies also collect royalties on behalf of scientists, for example when their paper is printed out and distributed to students. Anyone with publications to their name (and to which they own the copyright) can join a collecting society — though many people don’t, because of the misconception that it might be a scam. For those who do join, the rewards can be welcome: for example, each ALCS member received an average of around £450 this year.
The debate between physicists Niels Bohr and Albert Einstein over what quantum mechanics ‘really means’ has evolved into a long-standing myth, writes science writer Jim Baggott. Einstein rejected the possibility of some of the quantum weirdness implied by the theory, such as ‘spooky action at a distance’. Bohr’s ‘Copenhagen interpretation’ has been interpreted by some as ‘shut up and calculate’. But the idea that Bohr and his followers heavy-handedly imposed his view as a dogmatic orthodoxy doesn’t hold water, argues Baggott. In reality, “by the 1950s, the physics community had become broadly indifferent…. Quantum mechanics worked. Why worry about what it meant?” Nevertheless, the myth had a role in motivating the singular personalities that challenged it, laying the foundations for quantum computing.
Working as a scientist at an environmental non-profit organization can be similar to academic research, but requires a change of mindset: studies must always address real-world challenges. Jobs are usually advertised on job boards or LinkedIn, and it’s important for applicants to emphasize soft skills alongside scientific achievement. “It’s the same educational background and the same research, but just the way that I describe things had to shift completely,” says ecologist Kenneth Davidson. For early-career scientists who make the leap, non-profits can provide more job security and flexibility than academia.
Where I work

Matthew Nitschke is a senior research scientist at the Australian Institute of Marine Science, and a research fellow at Victoria University of Wellington, New Zealand.Credit: Giacomo d’Orlando for Nature
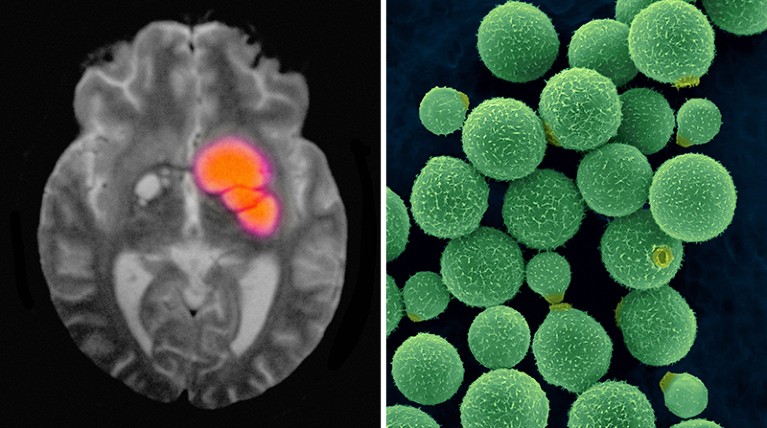
For ten years, Matthew Nitschke and his colleagues at the Australian Institute of Marine Science have been growing coral symbionts in the laboratory while gradually raising the heat. “Each time the symbionts adapt, we push the temperature up a bit,” says Nitschke. “They can now survive a constant 31 °C.” The goal is to develop corals able to survive waters warmed by climate change. “Studying marine conservation is hard,” says Nitschke. “Marine ecosystems are degrading. Coral reefs are bleaching: by 2060, without significant emissions reductions, mass coral bleaching on the Great Barrier Reef could be an annual event.” The next step is small-scale field trials out on the reef. (Nature | 3 min read)
Our award-winning ‘Where I Work’ series is now on display as a beautiful large-scale photography exhibition near the Nature offices in King’s Cross, London. If you’re near, do drop by (it’s free). Otherwise, check out the virtual exhibition online.
On Friday, Leif Penguinson was hiding among the lush mangroves in Ujung Kulon National Park, Indonesia. Did you find the penguin? When you’re ready, here’s the answer.
Thanks for reading,
Flora Graham, senior editor, Nature Briefing
With contributions by Katrina Krämer and Smriti Mallapaty
Want more? Sign up to our other free Nature Briefing newsletters:
• Nature Briefing: Microbiology — the most abundant living entities on our planet — microorganisms — and the role they play in health, the environment and food systems.
• Nature Briefing: Anthropocene — climate change, biodiversity, sustainability and geoengineering
• Nature Briefing: AI & Robotics — 100% written by humans, of course
• Nature Briefing: Cancer — a weekly newsletter written with cancer researchers in mind
• Nature Briefing: Translational Research — covers biotechnology, drug discovery and pharma
[ad_2]
Source Article Link