[ad_1]
A drug that uses messenger RNA technology has shown early success in addressing the core deficiency behind a rare genetic disorder. The results have ignited hope that the technology — which first gained attention through its breakthrough use in COVID-19 vaccines — could realize its long-awaited promise of generating therapeutic proteins directly in the body.
This clinical advance, reported today in Nature1, provides a boost to current mRNA applications, which remain limited to vaccines.
“This is a first step in the right direction,” says Katalin Karikó, a Nobel prizewinning pioneer of mRNA technologies who is affiliated with the University of Szeged in Hungary and the University of Pennsylvania in Philadelphia.
Yet challenges remain — especially the fleeting nature of mRNA and the side effects it causes, which complicate the path towards widespread adoption.
Metabolic makeover
Designed by Moderna in Cambridge, Massachusetts, the current therapy uses mRNA technology to restore metabolic function in people with propionic acidaemia.
This rare genetic disorder, which affects about one in 100,000 individuals worldwide, arises from mutations in either of two genes that together encode an enzyme necessary for the efficient breakdown of certain protein components. Without this enzyme, cells can’t process some nutrients properly.
That leads to the accumulation of toxic chemicals in the blood and tissues, and damages vital organs, including the heart and the brain. Symptoms, such as vomiting, usually start within the first few days after birth.
Why rings of RNA could be the next blockbuster drug
People can manage the condition with measures such as special diets. But there are currently no treatments that tackle the underlying cause directly.
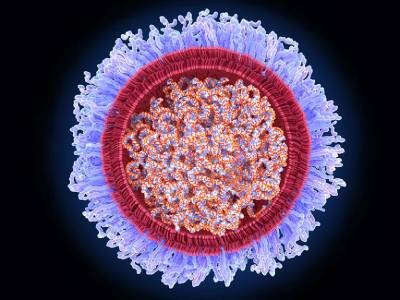
Moderna’s drug, known as mRNA-3927, aims to address that gap. It contains two mRNA sequences that each craft parts of the otherwise faulty enzyme. These mRNAs are encased in a tiny fat bubble — called a lipid nanoparticle — similar to the carrier used in the company’s COVID-19 vaccine.
The therapeutic mRNA drug is administered slowly through hours-long infusions every two or three weeks. It is also given in doses hundreds of times greater than those of COVID-19 vaccines. Once the therapy enters the bloodstream, the lipid nanoparticles help to direct the mRNA to cells in the liver, where the functional enzyme is made.
Trade-offs and benefits
Initial results from a small trial of mRNA-3927 indicate that the restoration of enzymatic activity is beneficial. Eight of the 16 participants had experienced life-threatening episodes connected to their impaired metabolism in the year before starting treatment. For those eight, the likelihood of experiencing another such event decreased by an average of 70–80% while taking the therapy.
This outcome, based on a small number of people, did not reach the threshold of statistical significance. Nonetheless, “it’s a very encouraging step”, says Jerry Vockley, a medical geneticist at the University of Pittsburgh Medical Center in Pennsylvania who helped to design the trial but who was not involved in its execution.
According to Kyle Holen, head of therapeutics development at Moderna, the company is now recruiting more trial participants as it advances mRNA-3927 towards the goal of marketing approval.
Moderna is also analysing other outcome measures related to quality-of-life metrics — indicators that, anecdotally at least, seem to be improving for some recipients of the treatment.
Nassrine Fawaz in Livonia, Michigan, has witnessed a transformation in her 4-year-old daughter, who has received mRNA-3927 for the past 2.5 years. After each infusion, “she’s focused, she’s energetic, she’s up and ready for the day — all of those great things”.
Room for improvement
Developers of mRNA therapeutics had long worried that repeated administration might trigger immune responses against the treatment. However, with individuals having now received regular infusions of mRNA for months or even years without issue, this concern has been alleviated.
“That’s pretty big,” says Alex Wesselhoeft, director of RNA therapeutics at Mass General Brigham’s Gene and Cell Therapy Institute in Cambridge, Massachusetts.
mRNA COVID vaccines saved lives and won a Nobel — what’s next for the technology?
But there are trade-offs: most people reported side effects in response to the treatment. These ranged from infections to severe swelling of the pancreas. However, as study investigator Andreas Schulze, a metabolic-disease specialist at the Hospital for Sick Children in Toronto, Canada, points out, many of the reactions are more likely to be “related to the underlying disease” than to the treatment.
Still, with a side-effect profile close to what Wesselhoeft describes as the “upper limit of tolerability”, and only modest clinical gains, he and others think that further refinements are needed before mRNA technologies can provide a fully corrective and long-term solution to genetic diseases.
“I’m just doubtful this is going to be a long-term therapy,” says Romesh Subramanian, a biotechnology consultant in Framingham, Massachusetts, who, in a previous job, worked in collaboration with Moderna scientists to develop mRNA therapies for rare diseases. “I think it needs to be much less frequent dosing with better [nanoparticles] or more potent mRNA.”
Meanwhile, many families affected by propionic acidaemia are maintaining a wait-and-see attitude. “The verdict is still out,” says Jill Chertow, founder and president of the Propionic Acidemia Foundation, a non-profit organization based in Deerfield, Illinois.
“We can only be hopeful since, right now, that’s all that we have.”
[ad_2]
Source Article Link