[ad_1]
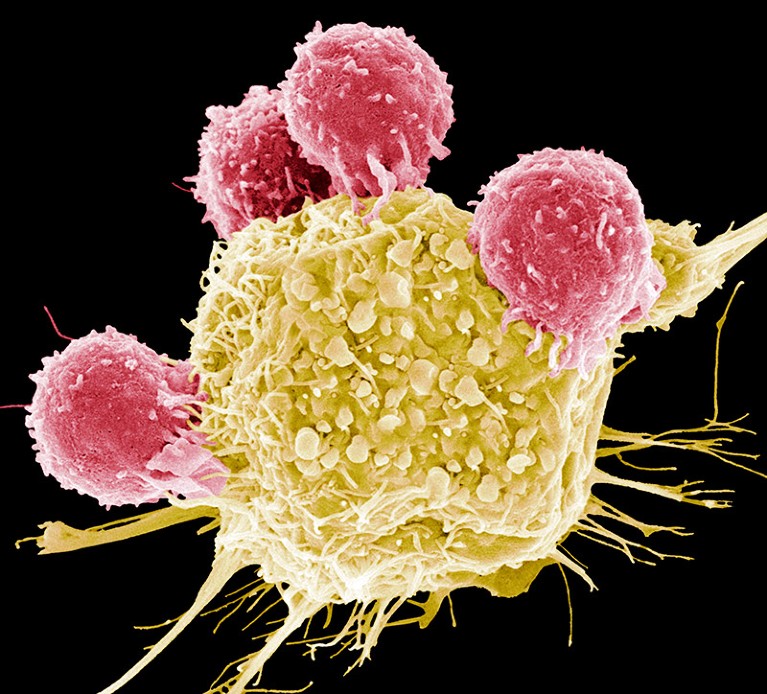
T cells (pink) attack a cancer cell (yellow) in this scanning electron micrograph image.Credit: Steve Gschmeissner/SPL
A small Indian biotechnology company is producing a home-grown version of a cutting-edge cancer treatment known as chimeric antigen receptor (CAR) T-cell therapy that was pioneered in the United States. CAR-T therapies are used mainly to treat blood cancers and have burgeoned in the past few years. The Indian CAR-T therapy costs one-tenth that of comparable commercial products available globally.
A single treatment of NexCAR19, manufactured by Mumbai-based ImmunoACT, costs between US$30,000 and $40,000. The first CAR-T therapy was approved in the United States in 2017, and commercial CAR-T therapies currently cost between $370,000 and $530,000, not including hospital fees and drugs to treat side effects. These treatments have also shown promise in treating autoimmune diseases and brain cancer.
India’s drug regulator approved NexCAR19 for therapeutic use in India in October. By December, ImmunoACT was administering the therapy to paying patients, and it is now treating some two-dozen people a month in hospitals across the country.
“It’s a dream come true,” says Alka Dwivedi, an immunologist who helped to develop NexCAR19 and is now at the US National Cancer Institute (NCI) in Bethesda, Maryland. Her voice becomes tender as she describes seeing the first patient’s cancer go into remission. These are people for whom all other treatments have failed, says Dwivedi. “They are getting cured.”
“It’s very positive news,” says Renato Cunha, a haematologist at the Grupo Oncoclínicas in São Paulo, Brazil. He says the Indian product could pave the way for making advanced cellular therapies accessible to other low- and middle-income countries. “Hope is the word that comes to mind.”
The product is also a reality check for researchers in high-income countries, says Terry Fry, an immunologist and paediatric oncologist at the University of Colorado Anschutz Medical Campus in Denver, who has advised the researchers involved in setting up ImmunoACT. “It lights a little fire under all of us to look at the cost of making CAR-T cells, even in places like the United States.”
Tremendous need
CAR-T therapy involves taking someone’s blood and isolating immune components known as T cells. These are genetically modified in the laboratory to express a receptor, known as a CAR, on their surface. This helps the immune cells to find and kill cancer cells. The engineered cells are then mass-produced and infused back into the patient, in whom they proliferate and get to work.
The race to supercharge cancer-fighting T cells
Data on demand for these therapies in India are limited, but one study looking at a specific form of leukaemia found that up to 15 people in 100,000 are diagnosed with the disease, half of whom relapse within two years of receiving treatment, such as chemotherapy, and who subsequently choose palliative care1. There is a “tremendous patient need”, says Nirali Shah, a paediatric oncologist at the NCI, who is also an academic collaborator of the researchers at ImmunoACT.
NexCAR19 is similar to its US counterparts, yet distinct in key ways. Like four of the six CAR-T therapies approved by the US Food and Drug Administration (FDA), it is designed to target CD19, a marker found on B-cell cancers2. However, in existing commercial therapies, the antibody fragment at the end of a CAR is typically from mice, which limits its durability because the immune system recognizes it as foreign and eventually eliminates it. Therefore, in NexCAR19, Dwivedi and her colleagues added human proteins to the mouse antibody tips.
Lab studies showed that the ‘humanized’ CAR had comparable antitumour activity to a mouse-derived one and induced the production of lower levels of proteins called cytokines2. This is important, because some people with cancer who receive CAR-T therapy experience an extreme inflammatory reaction known as cytokine-release syndrome, which can be life-threatening.
Trial data
Early-stage clinical trials for NexCAR19 in adults with different forms of lymphoma and leukaemia, showed that in 19 of the 33 people who received the therapy, the tumours had completely disappeared at the one-month follow-up3. The tumours in another four people had shrunk by half — achieving an overall response rate of 70%. Trial participants will be followed for at least five years.
“Whether this will hold or not is something only time will tell,” says Hasmukh Jain, a medical oncologist at Tata Memorial Centre in Mumbai, who led the trials.
Natasha Kekre, a haematologist at the Ottawa Hospital, points out that the results are based on a small number of participants with a range of blood cancers, which makes it difficult to assess the treatment’s efficacy for specific cancers.
Only two of the participants experienced more severe forms of cytokine-release syndrome, and none had neurotoxicities, another common but temporary side effect of CAR-T therapy.
The safety profile is better than that of some of the FDA-approved CAR-T treatments, says Kekre. This could be related to the product, as well as to years of the scientific and medical community learning how to better care for patients, she says.
Humanizing the CAR probably contributed to the therapy’s positive safety profile, says Rahul Purwar, an immunologist at the Indian Institute of Technology Bombay, and founder of ImmunoACT. But others say that link has yet to be established.
Fry says the setting and type of patient treated in India could also affect the results. “The toxicity profile of CAR-T cells is driven by a lot of other patient factors.”

A member of the ImmunoACT team preparing the NexCAR19 cancer treatment.Credit: ImmunoACT
Slashing costs
Although the treatment’s price tag is still high for many Indians, whose annual gross national income per capita is less than $2,500, NexCAR19’s cost offers hope that CAR-T therapy can be made more cheaply in other countries and contexts. To slash costs, the team developed, tested and manufactured the product entirely in India, where labour is cheaper than in high-income countries.
To introduce CARs to T cells, researchers typically use lentiviruses, which are expensive. Purchasing enough lentiviral vector for a trial of 50 people can cost up to US$800,000 in the United States, says Steven Highfill, an immunologist at the US National Institutes of Health Clinical Center in Bethesda, who has advised the Indian team. Scientists at ImmunoACT make this gene-delivery vehicle themselves.
The Indian team also found a cheaper way to mass-produce the engineered cells, avoiding the need for expensive automated machinery, says Highfill.
Patients’ costs are further reduced by the therapy’s improved safety profile compared with some of the other FDA-approved products, Purwar says. This meant that most patients did not need to spend time in intensive-care units.
Purwar hopes to further cut costs, including by scaling up production. ImmunoACT is planning to export the therapy to Mexico, and to develop new products, including a treatment for another form of blood cancer known as multiple myeloma.
But ImmunoACT faces competition. Several other Indian companies have launched local CAR-T trials, including Immuneel Therapeutics in Bengaluru, which has licensed technology developed by Spanish academics.
[ad_2]
Source Article Link